July 2022
This month’s political turmoil means the promised health disparities white paper has been delayed until post recess (best case scenario), if indeed it is ever even realised (worst case scenario). This is really disappointing given the opportunity it created to address the food and nutrition needs of infants and young children. However, other opportunities to shape early years diets for the better have arisen, and we have lots of interesting new reports, research, updated resources and more to share with you.
In ‘News’: two public consultations have just opened, one is the Scientific Advisory Committee on Nutrition’s draft report on feeding young children aged 1-5 years old, and the other a draft WHO guideline on the use of non-sugar sweeteners; the Food Foundation launched their 2022 Broken Plate report on the state of the nation’s food system and the Grocer released their 2022 infant and childcare report. We also share with you some new research relevant to eating well in the early years, and updates of our Eating Well in pregnancy guides and our Healthy Start and Best Start Foods Practical Guide.
In ‘Infant Milk news’ we have one new ‘growing up’ drink to highlight.
And lastly, we have no less than four forthcoming infant feeding-related events to highlight in case of interest.
Happy reading!
Please note as we’ll all be taking some time off in August, our next newsletter will be late September.
News
Open Consultations
SACN: Feeding young children aged 1-5 years - DRAFT
The Scientific Advisory Committee on Nutrition (SACN) has published a consultation on the draft report ‘Feeding young children aged 1 to 5 years’. The consultation is open for comment from 20 July to 16 September 2022 and interested parties are invited to draw SACN’s attention to any evidence that it may have missed. You can find more information in the link.
Once the report has been finalised we will share with you a summary of what recommendations have changed with respect to feeding of children aged 1-5 years, and will start updating our resources accordingly.
WHO Guideline on Use of Non-Sugar Sweeteners – DRAFT
The WHO have drafted these guidelines based on the results of an updated systematic review and meta-analysis of the health effects of the use of non-sugar sweeteners (which can be accessed here). The background is that efforts to limit free-sugars intake (the consumption of which have been linked to overweight and obesity, and other non-communicable diseases), have undoubtedly led to an increase in the popularity of non-sugar sweeteners. These low calorie/no calorie alternatives to free sugars are marketed as aiding weight loss or maintenance of healthy weight and are considered to be healthier (e.g. by the NHS Better Health brand its Food Scanner app). However, although individual sweeteners undergo toxicological assessment to establish safe levels of intake, there is no consensus on whether sweeteners are effective for long-term weight loss of if they are linked to other long-term health effects at habitual ‘safe’ consumption levels.
Key remarks from the online launch of the guidelines which took place on July 15th included the following:
“Efforts to reduce free sugars intake should be implemented in the context of achieving and maintaining a healthy diet. Because free sugars are often found in highly processed foods and beverages with undesirable nutritional profiles, simply replacing free sugars with non-sugar sweeteners results in a food or beverage in which any other unhealthy elements are mostly retained, and as a result the overall quality of the diet remains largely unchanged”.
“Replacing free sugars in the diet with sources of naturally occurring sweetness, such as fruits, as well as minimally processed unsweetened foods and beverages, will help to improve dietary quality and should be the preferred alternatives to foods and beverages containing free sugars”.
Drawing on the updated review of evidence, the WHO have developed the draft guidelines which are open for public consultation until August the 14th. To access the guidelines and submit your views, click here.
For our 2019 report on sweeteners in the diets of infants and young children (including recommendations which remain relevant given the WHO stance) see here.
If any organisation would like to liaise about our responses to these consultations please email vicky@firststepsnutrition.org.
Just launched
The Broken Plate 2022
The Food Foundation launched their annual report on the state of the Nation’s Food System on June 19th. The report examines ‘vital signs indicating the health of our food system, how it impacts on our lives and how we must change the food environment so that it delivers healthy and sustainable diets for everyone’. It highlights that unhealthy and environmentally unsustainable foods are now the norm, driving obesity and other diet-related disease, as well as climate change. After assessing ten key metrics providing an indication of the state of our food system and food environment, it outlines how changes are needed to make healthy foods more affordable, available and appealing. The report assesses whether policy is adequate to enable the progress needed in these three areas, and assesses six outcome metrics which reflect the impact that the food system is having on our health and environment and the impact that it will continue to have in the future if nothing changes.
The report and the annual initiative it is a part of is insightful and important. Improving the wider food environment and diets in general is essential for babies and young children whose diets are influenced by what their families eat. However, we have recommended to the Food Foundation that greater attention is given to what the under 5’s eat and why in their future analyses of the food system, so that appropriate actions can be recommended to improve their diets for the better. Babies are routinely being forgotten in wider food systems discourse in the UK (e.g. in the Government Food Strategy released in June, as explained here) and yet without improving diets in the first 1,000 days, the high rates of childhood obesity being observed will not be brought down.
You can read the Food Foundation’s Broken Plate 2022 report here.
The Grocer infant and childcare 2022 report
The Grocer published its infant and childcare 2022 report on June 16th. Interestingly given the content of previous years, it focuses on the ongoing inappropriate marketing of formula by industry asking “Will the tactics of brands prompt tougher rules?”. We hope so! In our opinion stronger regulations (at minimum, reflecting the International Code of Marketing of Breastmilk Substitutes and subsequent World Health Assembly Resolutions) are needed to protect parents and babies from misleading marketing, as well as meaningful enforcement of compliance with the regulations.
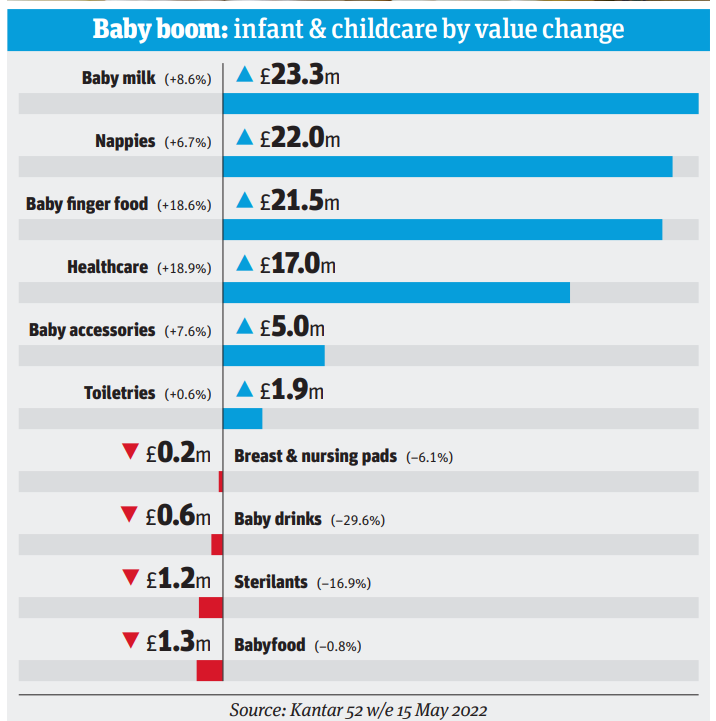
The report also states “Rising prices have helped the infant & childcare category grow in value on flat at volumes”. Indeed data within show that baby milk sales have grown in value 8.6% over the last year whilst volumes have only grown 6.7%, highlighting that the price increases we captured in our cost report update in April 2022 are clearly driving sales value gains. This is supported by the fact that branded baby milk value sales surged 9.7% while own label baby milk value sales fell 14.1%. There is only one own label infant formula, Mamia by Aldi, the price of which has only recently increased (to £8.49 per 900g, from £7.99 in April) whereas many branded products increased in price earlier in the year and by higher relative amounts.
In the midst of the cost of living crisis we remain concerned that infant formula prices may be unaffordable for many, especially with the Healthy Start payment amounts not keeping up with inflation, and we will continue advocating for appropriate actions.
New research
British Dental Association research on baby food pouches
The BDA recently researched the sugar content of baby food pouches marketed to infants and young children (‘Boutique’ baby food more sugary than Coca-Cola ‘rotting children’s teeth’ (telegraph.co.uk)). Results were alarming, with pouches containing up to 5 times as much sugar per 100g as Coca Cola. The full results of the research, including details on specific items, can be found here. They reveal that the highest levels of sugar are found in the ‘boutique’ brands such as Ella’s Kitchen and Annabel Karmel.
Although parents are led to believe that commercially-produced fruit and vegetable-based purées are appropriate ‘first foods’ for infants, they are often high in the free sugars associated with dental decay; the primary reason for hospital admissions in young children in the UK. In addition, the foods infants are exposed to at an early age have long-lasting effects on their liking of specific tastes as infants learn to recognise the flavours, texture and appearance of individual fruits and vegetables. Evidence suggests that feeding infants bland, sweet, highly processed purées may lead children to develop fussy eating patterns, rejecting healthy family foods in favour of highly processed foods, one of the causes of overweight, obesity and other chronic diseases later in life.
As we reported in our 2017 review of UK baby foods, processing fruits and vegetables into a puréed form may also promote over-consumption, as the energy density and physical structure of foods is altered, impacting on satiety and energy intake. Additionally, puréed foods are smoother than their unprocessed or minimally processed counterparts and so can be rapidly swallowed, making it more difficult for care-givers to know when their infant has had enough to eat.
Unfortunately, the clever but inappropriate marketing on baby food pouches we highlighted in 2018 still persists, and the numerous misleading health and nutrition claims make it hard for parents and carers to make informed choices on what to feed their children. Here are some of the misleading claims documented by the BDA survey, and the evidence or public health guidance refuting these claims:
Suitable for children 4m+ – The NHS recommends introducing solid foods from around 6 months of age when the baby is showing signs of developmental readiness
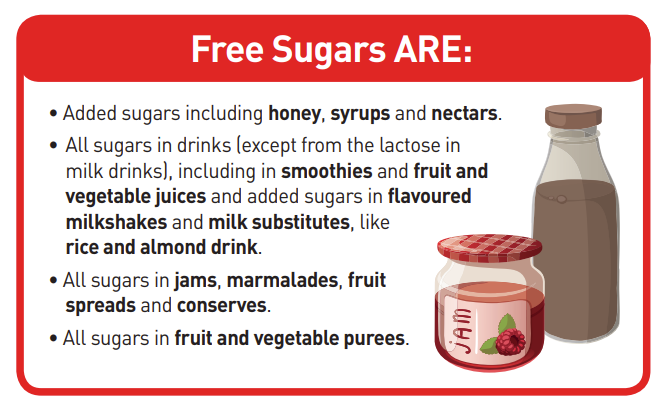
Only contains naturally occurring sugars / no added sugar – All free sugars, regardless of source, are associated with dental caries and weight gain. This includes sugars “naturally present in fruit and vegetable juices, purées and pastes and similar products in which the structure has been broken down”. Action on Sugar have produced a helpful guide on how to identify the free sugar content of foods which can be accessed here.
Nutritionally approved / in line with infants nutritional and developmental needs – the UK Government’s Scientific Advisory Committee on Nutrition recommend that the average intake of free sugars should not exceed 5% total dietary energy intake for young children over 2 years of age. This equates to a maximum of 13g per day for girls aged 2-3 years and 15g per day for boys of the same age. Roughly 60% of the pouches surveyed by the BDA contain enough free sugar to exceed the maximum daily intake for girls aged 2-3 years if two pouches were consumed in a day, and a further 10% exceeded the maximum intake among this age group in a single pouch.
High in fibre/contain one of your five a day – although intact fruits and vegetables are a good source of fibre and vitamins, processing may result in changes in the quantity and bioavailability of nutrients and phytonutrients in foods. The evidence we reviewed for our 2018 report on baby food purées suggests that the processing techniques required to produce baby foods are linked with losses of total fibre, glucosinolates and heat-sensitive nutrients such as vitamin C.
It is also important to note that on-pack instructions to “eat straight from the pouch” are against NHS guidance. Sucking from the pouch increases the risk of dental decay, does not allow children to see the food they are eating, does not allow infants or care-givers to know how much they are eating and changes eating from a chewing to a sucking experience.
We support the BDA’s call for action to tackle the inappropriate marketing of baby food pouches, which needs to be a part of efforts to prevent the inappropriate marketing of all formula, foods and drinks aimed at infants and young children, in order to protect the short and long-term health of this vulnerable group. We await the promised Government consultation on the marketing and labelling of baby foods.
See our Eating Well: the First Year guide on introducing solids and eating well up to baby’s first birthday for evidence-based and conflict-free information and practical advice on feeding babies.
A content analysis of ‘junk food’ content in children’s TV programmes: a comparison of UK broadcast TV and video-on-demand services
Barker and colleagues report on and compare the results of two content analyses of high in saturated fat, sugar or salt (HFSS) food imagery, one of popular UK children’s TV channels (for pre-school children and older) and the other of a selection of children’s programmes available on video-on-demand (VOD) services. They found HFSS images to be common on the kids TV and the VOD services and state that this is likely having an effect on HFSS consumption in children, therefore being one driver of overweight and obesity.
The authors urge Ofcom to consider the implications of allowing children to be exposed to HFSS content through programme content and to put regulations in place to prevent this from happening. They also recommend that the DHSC considers whether the current plan to ban ‘junk food’ adverts before the 9 p.m. watershed goes far enough to prevent exposure to HFSS content, and to consider HFSS content in programmes broadcast before this time.
Read the full paper here.
Trends in use of specialized formula for managing cow's milk allergy in young children
Co-authors Mehta and Allen and colleagues undertook a cross-sectional analysis of national prescription databases in the UK, Norway and Australia and examined volume and cost of specialised formula, and the proportion of infants prescribed specialised formula. Expected volumes assumed 1% cow's milk allergy incidence and similar formula feeding rates between infants with and without milk allergy.
Results from England were that prescribed volumes of specialised formula for infants rose 2.8-fold from 2007 to 2018, with similar trends in the UK. In 2020, total volumes were 9.7- to 12.6-fold greater than expected and specialised formula for infants cost the equivalent of 103 euro per birth. In 2020, 30%–50% of prescribed specialised formula across the three countries was amino-acid formula.
The authors conclude that in England (as well as Norway and Australia), specialised formula prescriptions have increased in the early 21st century and exceed expected levels, and that unnecessary specialised formula use due to overdiagnosis may make a significant contribution to free sugars consumption in young children.
Read the full paper here.
For independent information about the specialised formulas being marketed in the UK for infants with cows’ milk and other allergies, see our specialised milk report.
The “Cinderella sector”: The challenges of promoting food and nutrition for young children in early years’ settings in England
This paper by Warren, Williams and Knai points out that the quality of food that children eat in early childhood has profound impacts on their future wellbeing, and that many young children eat most of their food whilst at nursery or a childminders. The paper highlights that Ofsted includes a welfare requirement that early years settings (EYS) provide food and drink that are ‘healthy, balanced and nutritious’ but that despite this requirement there are no mandatory standards for assessment. The research involved interviewing various stakeholders about food provision in EYS in England, the use of the voluntary food and drink guidelines and the effects of government support on the early years’ sector. Those consulted felt insufficiently consulted, under-valued, lacking in support and underfunded. Some EYS had never heard of the voluntary food and drink guidelines or did not use them. There was disagreement about the role and effect of the voluntary standards, but most believed that they should be made compulsory for a range of reasons, including establishing healthy food preferences and food-habits, reducing the burden of childhood (and related adulthood) obesity, providing consistency across the sector, enabling EYS to feel more confident in interpreting the EYS food and drink requirements, and improving equity.
Read the full paper here.
Updated Eating Well guides
We have updated our Practical Guides “Eating well in pregnancy: A practical guide to support teenagers”, “Eating well for a healthy pregnancy” and “Healthy Start Best Start Foods A practical guide” and they are available on our website here. Edits to all three resources now reflect the most recent changes to the Healthy Start scheme and include Best Start Foods (Scotland) and changes in contact details of relevant organisations. Other changes are outlined below.
“Healthy Start and Best Start Foods A practical guide” explains the Healthy Start scheme in England, Wales and Northern Ireland, and the Best Start Foods scheme in Scotland, and how families eligible for these schemes can be supported. It has been updated to take in to account the digitization of the scheme, the change in the payment amounts and other changes to the schemes. The resource gives examples of how the food payments can be spent (and takes in to account recent food price increases), with recipes and advice for health professionals who support families in their areas.
“Eating well for a healthy pregnancy” aims to enable health professionals to support pregnant women to better understand their food and nutrition needs in pregnancy and how best to meet them. It was updated in February 2022 so the current changes are minimal and mostly relate to changes in the Healthy Start and Best Start Foods schemes.
“Eating well in pregnancy: A practical guide to support teenagers” aims to enable health professionals to support pregnant teenagers to better understand their additional food and nutrition needs and how these needs might best be met. It includes recipes and meal ideas and can sit alongside other local public health guidance to provide a practical explanation of what 'eating well' looks like.
The main updates that have been made are around the advice on foods to limit or avoid during pregnancy, which are now in line with recent changes to NHS advice, and tips for eating well out of the home now better recognise the increasing contribution of home food delivery to many pregnant women’s diets.
Infant Milk News
New products
SMA Little Steps Plantygrow
Nestlé have recently launched a plant-based milk alternative “growing-up” drink for 1-3 year olds. This is now the second plant-based milk alternative growing-up drink available in the UK, the other being Alpro soya growing-up drink. The product is branded as part of the Little Steps sub brand which has now grown to include cows’ milk-based formula milks, Plantygrow plant based growing-up drinks and a range of finger foods and cereals for toddlers from 12 months +.
The main ingredients in Plantygrow are water, hydrolysed flour from wheat, oat, barley and rye, maltodextrin and vegetable oil. As there are no specific compositional, marketing or labelling regulations for either growing-up milks or plant-based milk alternatives, their composition is highly variable and they may have limited nutritional equivalence to animal milks. Although manufacturers of plant-based growing-up drinks recommend their products as suitable for young children, this evaluation is entirely their own.
In the UK, public health guidance is that unsweetened, fortified milk alternatives, but not those that are rice based, can be included as the main milk drinks from the age of 1 year. It is important however, to note that there are some issues related to the macro and micronutrient content of plant-based milks and the bioavailability of the fortificants added. Plantygrow has a greater energy content than many plant based milk alternatives on the general market but is lower in protein and contains added free sugars.
Families should be made aware that young children require an energy and nutrient dense diet, and that perceived health benefits of a plant-based diet may not be relevant or health promoting for young children. You can find a broader discussion on issues related to the use of plant-based milks in young children’s diets in our briefing paper: Plant-based milk alternatives in the diets of 1–4 year-olds
Plantygrow is marketed as a “growing-up” drink, and like cow’s milk based “growing-up” and “toddler” milks, it is an ultra-processed food with added free sugars; in Plantygrow the free sugar added is maltodextrin. This is of concern as the taste profile of sweetened, ultra-processed foods does not accustom young children to the real taste of the unprocessed and minimally processed foods recommended as the basis of a healthy diet during childhood. The NHS and the European Food Safety Authority say that growing up and toddler milks are not a necessary part of a young child’s diet.
Given the current cost of living crisis, a particularly pertinent feature of Plantygrow is that it is expensive. Plantygrow retails at 75p per 200ml and Nestlé recommend 2x200ml per day. Feeding a young child 400ml a day as recommended by the manufacturer would cost parents £10.50 per week or £45 per month. This compares to £2.80 per week and £12.00 per month should an equivalent amount of supermarket own brand unsweetened fortified, soya milk be used. There are implications for both the diet of the toddler and the rest of the family if expensive unnecessary products are purchased which reduce the amount of household income available for buying healthier staples for the family. For a broader discussion about the use of milks marketed as “growing-up” and “toddler” milks in the diets of young children see our briefing paper: Drinks for young children marketed as ‘growing-up’ and ‘toddler milk’.
Looking for information about infant milks? Check out our website www.infantmilkinfo.org. Still got questions about infant milks? Contact susan@firststepsnutrition.org
Forthcoming
World Breastfeeding Week – 1st-7th August 2022
WABA are running the annual World Breastfeeding Week campaign, with this year’s theme being ‘Step up for breastfeeding – educate and support’. The campaign aims to strengthen the warm chain of support for breastfeeding by improving the capacity that healthcare, community and workplace actors have to protect and promote breastfeeding-friendly environments in a post pandemic world. WABA invite all of us to identify our role in the warm chain and understand how we can protect, promote and support our role using their resources. More information can be found here.
We look forward to seeing everyone’s social media coverage using #WBW2022 #WorldBreastfeedingWeek2022
UNICEF Baby Friendly conference November 23rd-24th 2022
A reminder that an *early discount is still available until the end of August* for this year’s Baby Friendly Annual Conference (Virtual) which will take place over two days, the 23rd and 24th of November 2022. There will be in-depth updates on recent research and innovations related to infant feeding and relationship building, live Q&As and virtual posters. Interactive new networking opportunities will also be made available so delegates can catch up between talks and after the conference. The speaker line up covers a broad range of topics, and includes our Director, Vicky Sibson:
Latest updates on Sleep Safety and ‘Sleep, Baby & You’ – Professor Helen L. Ball, Professor of Anthropology & Director, Durham Infancy & Sleep Centre, Durham University
Compassionate care: compassionate leadership – Sheena Byrom, Midwife, Director, All4Maternity
How the marketing of formula milk influences our decisions on infant feeding – Nigel C Rollins, Scientist, World Health Organization
Ultra-processed foods – Vicky Sibson, Director, First Steps Nutrition Trust
Booking closes at 5pm on November 18th.
Find out more and book tickets for the UNICEF Baby friendly 2022 conference here.
WHO and BMJ webinars on “the problem with the formula milk industry”
Following on from the WHO and partners two revealing reports on the ongoing problem of inappropriate marketing of breastmilk substitutes by the baby food industry (as reported on in our February and April newsletters), the WHO and the BMJ are convening two webinars in September about “the problem with the formula milk industry”. The first 'An Unhealthy Influence on Health Professionals?' on September 8th will be facilitated by Dr Chris van Tulleken and will have speakers from Saatchi World Services and WHO, reflections from a range of health professionals and a series of propositions about what can be done.
Register for the event here.
The Association of Breastfeeding Mothers annual Virtual Conference on the 17th September 2022
The ABM are hosting their third Virtual Conference in the autumn, promising a line up of speakers covering a topics including: Supporting the Allergy Dyad, Breastfeeding Through Medical Complexity, Colonisation and Artificial Milk, Why Cultural Safety in Breastfeeding Matters and Body Work and Infant Feeding - An IBCLCs Perspective. You can get tickets here.