November 2022
Welcome to our November newsletter. We hope you’re beginning to feel festive and have some nice plans for the forthcoming holidays.
This month we share with you the latest data on childhood obesity, a summary of the Food Active conference which is relevant in this regard, some advice on the use of rice and rice-based products in the diets of infants and young children, and also on supporting formula-feeding families in the event of a planned power cut.
We have a lot of ‘Infant Milk news’ for you, with several discontinued products, some new more economic formula pack sizes, and an update of our infant milk cost report.
As secretariat of the Baby Feeding Law Group (BFLG) UK, we highlight a news article arising from a presentation by Dr Nigel Rollins at last week’s the Unicef Baby Friendly conference, “How the marketing of formula milk influences our decisions on infant feeding”. We also share an update on our forthcoming report on infant milks marketed as foods for special medical purposes.
Lastly, we hope that we may have the opportunity to meet some of you at two forthcoming events: a meeting of the APPG on Infant Feeding and Inequalities on Tuesday December 6th and the iHV leadership conference in London on December 7th.
We will not be sending a newsletter in December so wish you all a Merry Christmas, however you choose to celebrate, and best wishes for a happy New Year. Our next newsletter will be sent to you in late January 2023.
News
Latest data from the Government's National Child Measurement Programme
The most recent findings from the Government's NCMP for England were published on 3rd November. Launched in 2005/06, the programme provides data on the number of children in Reception (aged 4-5 years) and Year 6 (aged 10-11 years) in mainstream state-maintained schools in England living with overweight and obesity. The results for the 2021/22 school year can be found here.
The news is somewhat positive, as the prevalence of reception-aged children living with obesity has decreased from 14.4% in 2020/21 (during the covid-19 pandemic) to 10.1% in 2021/22. However, rates of obesity and overweight in young children remain unacceptably high. An analysis of trends among reception aged children reveals that, although rates of children living with severe obesity have decreased since 2020/21, they remain higher than their pre-pandemic levels. Furthermore, the most deprived children are disproportionately affected. In 2021/2022, children in the most deprived areas were more than twice as likely to be living with obesity compared to those living in the least deprived (13.6% compared to 6.2% respectively), a difference which has widened by 1.3% since 2013/14.
As the cost of living continues to rise, this is particularly worrying news for infants and young children living in the most deprived households in England, especially as latest data shows that nearly one in five families in the UK are now food insecure, and close to a half of food insecure households reported decreases in dietary quality, which are both known risk factors for overweight and obesity.
Greater efforts to prevent excess weight gain during the first years of life (particularly among the most disadvantaged), are necessary to ensure children arrive at school a healthy weight.
Our 2021 report, Enabling children to be a healthy weight, outlines what a journey which promotes a healthy weight in the early years would look like, and what actions we believes need to be funded and implemented in England, to achieve this.
#Foodactive2022 - Prioritising child healthy weight in an age of crises
Earlier this month, Food Active held their annual conference, bringing together leaders in child health to reflect on the impacts of the covid-19 pandemic, and to consider learning that could inform the current cost of living crisis. A full recording of the conference can be found here.
The importance of safeguarding the health of UK children during crises was highlighted, informed by data from the covid-19 pandemic which showed significant increases in the prevalence of overweight in young children and widening disparities in the nutritional status of children from the most and least deprived households. The speakers outlined how the social and economic factors that contributed to child health disparities during the covid-19 pandemic remain unchanged. Cuts to public health budgets and services, an increased number of households at risk of income poverty, and the government withdrawal of policies to tackle overweight and obesity are some of the factors leaving children at risk of poor health in the short-term and long-term.
A “whole systems approach” was presented as a helpful framework to understand the wider conditions that impact on child health and can be used to inform multisectoral actions to tackle overweight and obesity in children. More information can be found here, alongside a range of resources launched at the conference, to provide evidence, information and tools to help promote healthy weight across the life cycle.
Infants and young children are not being considered systematically in discussions about food security as the cost of living continues to rise, and in our opinion they need to be. We will be updating our Cost of Living briefing and asks iminently, and continue advocating across the sector for the unique needs and vulnerabilities of infants and young children to be better taken in to account.
Baby rice and rice-based products for babies
Over the last few weeks, we have received a flurry of enquiries from healthcare professionals, the catering sector and parents related to arsenic in rice and rice-based products for babies and young children.
Inorganic arsenic, which is the form of arsenic that poses a risk to health, occurs naturally in the environment and is therefore present in the food we eat. Rice takes up more arsenic from the environment than other cereal crops which is why it is a greater cause for concern. Long term exposure to high levels of arsenic causes skin lesions and may be a precursor to skin cancer (WHO, 2018). Although arsenic can’t be eliminated from food and we are all exposed to it to some degree, the concentration of arsenic in rice-based foods is regulated. New regulations, introduced by the EU in January 2016, set out maximum concentrations of inorganic arsenic permissible in rice and rice-based products, with stricter limits for rice destined for the production of foods and drinks marketed for infants and young children.
We are not aware of any independent monitoring of or any robust reports on the arsenic content of rice-based foods made for babies or young children since the regulatory changes in 2016. One report on the arsenic content of rice in the UK suggests that about 50% of the rice samples collected would not be suitable for baby food production (Menon et al, 2020). However, there is no evidence to imply that this rice is used in the production of baby foods.
The Food Standards Agency (FSA) states that rice can be consumed as part of a healthy, balanced diet, but, as a precaution, advises that rice-based milk alternatives should not be given to children under the age of 5 as a substitute for breast milk, infant formula and cows’ milk. This includes rice-based infant formula and follow-on formula. The rationale for the recommendation is that compared to other consumers, infants and young children tend to drink more milk and their lower body weight means their relative exposure to arsenic from rice-based milk alternatives is higher. Although it is possible to buy rice-based formula milk online, UK law does not permit its sale. You can find out more about alternative plant based milks for young children in our briefing paper: Plant-based milk alternatives in the diets of 1–4 year-olds.
A common-sense approach to the question of how to safely approach rice and rice-based products in the diets of infants and young children would be to ensure that they are only offered in moderation. Our Eating well guides – Eating well: the first year and Eating well: vegan infants and under-5’s - provide practical examples of how to do this, incorporating rice and rice-based products alongside a range of other grain and cereal based foods as part of the complementary diet and beyond. Eating well: snacks for 1- to 4-year-olds shows examples of snack options, including rice cakes, that can be taken out and about (noting that babies under 1 year old do not need any snacks). Whilst rice-based milk alternatives should not be offered as a substitute for breast milk, infant formula and cows’ milk, using rice milk in moderation in recipes should not pose a risk to infant health.
Planned power cuts and advice on safer formula feeding
Given news reports of possible planned power cuts in January and February, we wanted to provide some initial and headline advice for those of you working with families feeding their babies formula. You may want to encourage them to think ahead about how they would safely prepare their babies feeds in the event of such power outages.
The good news is that, at the moment, it appears that outages will be planned and will last no more than 3 hours, between 4 and 7pm. This means that the NHS advice on formula feeding away from home should be suitable:
If using a vacuum flask, it is important to fill it up to the top to ensure the water stays hot (you can read more about this in our FAQ about making up formula away from home here).
If using a ready to feed formula, it is important to note that these are much more expensive than powdered formulas. You might want to remind families that in terms of the nutritional composition (and as for powdered infant formula), there is no difference between brands despite price differences (which are shared in our cost report). It is also important to follow instructions for the safe disposal of unused formula. In short, unfinished bottles should be discarded after a feed, and opened products which have not been used should be discarded if not refrigerated (as will be the case in a power cut).
Finally, families may wish to contact their energy provider to see if they can get on their “Priority Service Register” in order to receive pre-warnings about planned power outages and to find out what other support they can offer.
We hope you can find all the answers to queries about infant milk safety on our Infant milk info website, here: Questions about infant milk safety and if not please feel free to email us: vicky@firststepsnutrition.org.
Infant Milk News
New Products
Danone have now introduced ‘Big packs’ of Aptamil First Infant Milk and Follow-on Milk. These 2 x600g packs would be expected to last 50% longer than the standard 800g can and, on the basis of cost per gram, are less expensive than the equivalent standard packs.
Discontinued Products
All discontinued products this month are follow-on milks. Although follow-on milk is not recommended by the NHS and offers no nutritional benefits to infants compared to infant formula, parents who used these products and wish to continue using follow-on milk will need to find alternatives.
Danone have discontinued Aptamil ready-to-feed Follow-on Milk and Cow & Gate ready-to-feed follow-on milk in 1 L bottles.
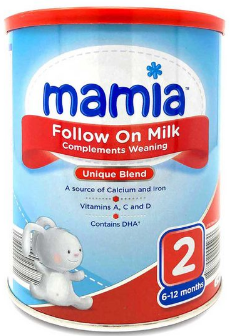
Aldi have now discontinued their Mamia follow-on milk. This was the least expensive follow-on milk on the UK market.
Cost of Infant milks
Our report ‘Costs of infant formula, follow-on formula and milks marketed as foods for special medical purposes available over the counter in the UK’ has been updated and can be accessed at infantmilkinfo.org/costs. Although the weekly cost of feeding a 2–3-month-old baby the most or least expensive powdered infant formula has remained reasonably stable since our last report in April 2022 at £21.25 per week and £7.73 per week respectively, it will come as no surprise that there have been some significant price increases across all types of formula and at all price points in between these figures. Over the last seven months, price increases have affected mainly Danone products (Aptamil and Cow & Gate), which have risen by up to 9%. This is significant as Danone dominates the infant milk market, holding 76% of the market share in 2021 (Mintel, 2022).
For those eligible for the Healthy Start scheme (in England, Wales and Northern Ireland), families with one infant receive a healthy food allowance worth £8.50 per week which is equivalent to 2x £4.25 healthy start payments. Unfortunately, this no longer covers the cost of a 900g can of the least expensive infant formula on the market, Aldi’s Mamia, which is now £8.59. (In Scotland, the Best Start Foods scheme payments are worth £9/week for eligible families with babies under 1, meaning this formula can be purchased without the family needing to add a contribution).
For families who cannot access the Aldi formula, the least expensive of the more widely available alternatives (on the basis of a week’s average consumption), now cost between £8.99 and £11.00 per can. Healthy Start beneficiary families using these products now need to find from their other income sources, the additional 49p to £2.50 for each can purchased (or up to £2 for Best Start beneficiaries).
'Big packs' of formula are less expensive per 100ml than standard pack sizes. However, purchasing a larger pack will require families to pay a greater up-front cost, and these packs are not available in all retail contexts.
As the Chancellor’s Autumn Statement did not include Healthy Start in the list of benefits that would be uprated from April 2023, we will continue to support calls for Healthy Start allowances to be increased (alongside other improvements) to ensure that the scheme can better act as the nutritional safety net it is meant to be.
Watch out for more in depth analysis of infant milk cost trends which will be included in our updated Cost of Living briefing.
Looking for information about infant milks? Check out our website www.infantmilksinfo.org. Still got questions about infant milks? Contact susan@firststepsnutrition.org
Baby Feeding Law Group UK news
Milk formula firms target women looking for pregnancy advice
On 27 November, the Observer shared some key highlights from Dr Nigel Rollins’ presentation from the UNICEF Baby Friendly annual conference, held last week. The piece by Rosie Taylor highlighted how manufacturers of commercial milk formula use sophisticated algorithms to target advertising of milk formula on digital platforms (including social media) to women whose online behaviour suggests they may be pregnant.
Since infant formula advertising is prohibited in the UK, Dr Rollins shared research demonstrating how companies use loopholes to provide information to pregnant women, mothers, and parents, including promoting brands through sponsored social media posts (on Facebook, Twitter, and Instagram), through the development and promotion of company apps, online “baby clubs”, helplines offering advice and various other strategies. This information comes from reports shared by the WHO this year on the Scope and impact of digital marketing strategies for promoting breast-milk substitutes and How the marketing of formula milk influences our decisions on infant feeding.
Nigel Rollins’ presentation and this news article again remind us how UK laws on the marketing of breastmilk substitutes need to be urgently strengthened, in line with the International Code of Marketing of Breastmilk Substitutes and all subsequent World Health Assembly resolutions, to better protect families from undue commercial influence on how they feed their babies.
Update on our forthcoming report: Infant milks marketed as foods for special medical purposes (FSMP) - The case for regulatory reform to protect infant health
This upcoming report sets out the case for the strengthening of UK law around the marketing of infant milks marketed as foods for special medical purposes (iFSMP). It addresses serious issues arising from shortcomings in the current law and examines the exploitation and misuse of this regulatory category by commercial milk formula companies, which undermine breastfeeding and threaten the health of babies who are not fully breast(milk)fed. It explains why, without independent expert monitoring of company compliance with the law, these issues will not be resolved, and recommends government actions to address these issues, most notably, by embedding the International Code of Marketing of Breastmilk Substitutes and all subsequent World Health Assembly resolutions into UK law.
We have now finalised this report and plan to publish it in early December, so please keep watch on our Twitter feeds and Facebook if you’re interested.
Forthcoming
APPG on Infant Feeding and Inequalities Meeting: Tuesday 6th December
The All-Party Parliamentary Group on Infant Feeding and Inequalities will be hosting a hybrid meeting on the 6th of December at 1pm. First Steps have a slot on the agenda, and Maiko Kamara and Katie Perira-Kotze will be presenting “A report on the labelling of infant formula and follow-on formula in the UK, and companies' adherence to UK laws and Guidance Notes, and the International Code of Marketing of Breast-milk substitutes." If you are interested in attending this meeting (which is open to anyone), you can sign up for updates and the Zoom link via this form and visit the APPG website.
iHV conference ‘Translating vision in to reality: London, December 7th
Our Director Vicky, and nutritionist Rachel, will be exhibiting at this iHV conference in London next month. We will be sharing our work and resources with health visitors and hope to receive feedback to improve the work we do towards our objectives, which includes providing resources for health workers to support them in their work with pregnant women and young families. Please do come and meet us in person. For more information please click here.